As medical leaders, we are all too familiar with the effects of burnout and compassion fatigue. The physical, emotional, and mental toll of providing care to others can be immense and overwhelming. Fortunately, there are ways to maximize clinician well-being in order to reduce burnout and promote healthier outcomes for those on the front lines of healthcare.
This blog will discuss six strategies at the unit level for maintaining mental health while working in a challenging environment: fostering a positive work environment; implementing structured debriefings; utilizing peer support networks; developing meaningful professional connections with colleagues; encouraging self-care practices; and addressing systemic issues that impact clinician burnout. Read on to learn more about these strategies!
1. Fostering a Positive Work Environment
The healthcare industry can be a demanding and stressful field for those who work within it. That’s why it is essential to foster a positive work environment that supports the well-being of healthcare workers. A positive work environment can lead to better mental and physical health outcomes for employees, increased job satisfaction, and improved patient care.
A work environment that promotes positivity could involve setting clear communication expectations, recognizing employee accomplishments, or promoting employee wellness programs. By implementing these strategies, healthcare organizations can build a culture that prioritizes the well-being of employees and ultimately delivers better outcomes for patients.
2. Implementing Structured Debriefings to Process Difficult Experiences
In healthcare, processing difficult experiences is essential for team member well-being and for improving patient outcomes. One strategy that has gained popularity is implementing structured debriefings. These debriefings provide a safe space for team members to discuss and reflect on challenging experiences. Research has shown that implementing structured debriefings has led to improved team communication, increased job satisfaction, and reduced burnout.
By providing a framework for meaningful discussion, structured debriefings allow team members to process emotions and improve their ability to handle similar situations in the future. As healthcare professionals, it is crucial to prioritize addressing difficult experiences through effective strategies like implementing structured debriefings.
[RELATED: Org Wellness Structure Roadmap: A visual structure to help organize your teams]
3. Utilizing Peer Support Networks to Promote Resiliency and Stress Management
Research has shown that clinician peer support networks can be an extremely effective tool in promoting resiliency and managing stress in healthcare professionals. The demanding nature of their work can take a toll on clinicians both professionally and personally, but having a supportive network of colleagues can make all the difference.
These networks can provide a safe space for clinicians to discuss their experiences and emotions, as well as share coping strategies that have worked for them. By prioritizing the mental health and well-being of healthcare professionals, we can ensure that they are better equipped to provide high-quality care to their patients. As healthcare continues to evolve, it’s important that we recognize the importance of clinician peer support networks as a valuable resource for promoting resiliency and stress management.
4. Developing Meaningful Professional Connections with Colleagues
Developing meaningful professional connections with colleagues is essential in any workplace. Research has shown that individuals who have positive relationships with their colleagues are more engaged, productive, and satisfied at work. Moreover, having strong connections with others can provide opportunities for learning, professional growth, and support during challenging times.
While building these connections may require time and effort, the benefits are worth it in the long run. By being approachable, respectful, and actively listening to others, individuals can foster positive relationships with their colleagues. Furthermore, taking advantage of networking events, mentoring programs, and other professional development opportunities can help individuals expand their social circle and build new connections. Ultimately, investing in professional relationships can lead to a more fulfilling and successful career.
5. Encouraging Self-Care Practices That Enhance Mental Health Outcomes
As medical professionals, we often place the health and wellness of others before our own. However, neglecting self-care practices can result in negative effects on our mental health, ultimately affecting our ability to provide quality care for our patients. Research has shown that implementing self-assessment tools and other evidence-based practices can have a significant impact on mental health outcomes for medical professionals. By taking the time to prioritize our own well-being, we can better serve our patients and lead by example for our colleagues.
What are the benefits of mental health self-assessment?
Mental health self-assessment can provide medical professionals with an opportunity to better understand their personal strengths and weaknesses, as well as identify areas of improvement. By taking the time to reflect on our mental health, we can become more aware of potential stressors and take steps to address them. Additionally, these assessments can help clinicians monitor changes in their mental health over time, allowing them to make timely interventions and prevent further deterioration. Ultimately, this practice can equip clinicians with the necessary skills to manage stress and maintain positive mental health outcomes.
Ultimately, incorporating these strategies into our everyday practices is key to ensuring clinician well-being and improving mental health outcomes in healthcare professionals.
6. Addressing Systemic Issues that Impact Clinician Burnout and Compassion Fatigue
Clinician burnout and compassion fatigue are significant problems in the healthcare industry, with an estimated 50% of clinicians experiencing burnout. Systemic issues are often cited as the root cause of these challenges, including high-stress levels, limited resources, and administrative burdens. Fortunately, there is a growing body of evidence-based practices and interventions that can be implemented to address these concerns.
What is the first step to addressing systemic drivers of distress?
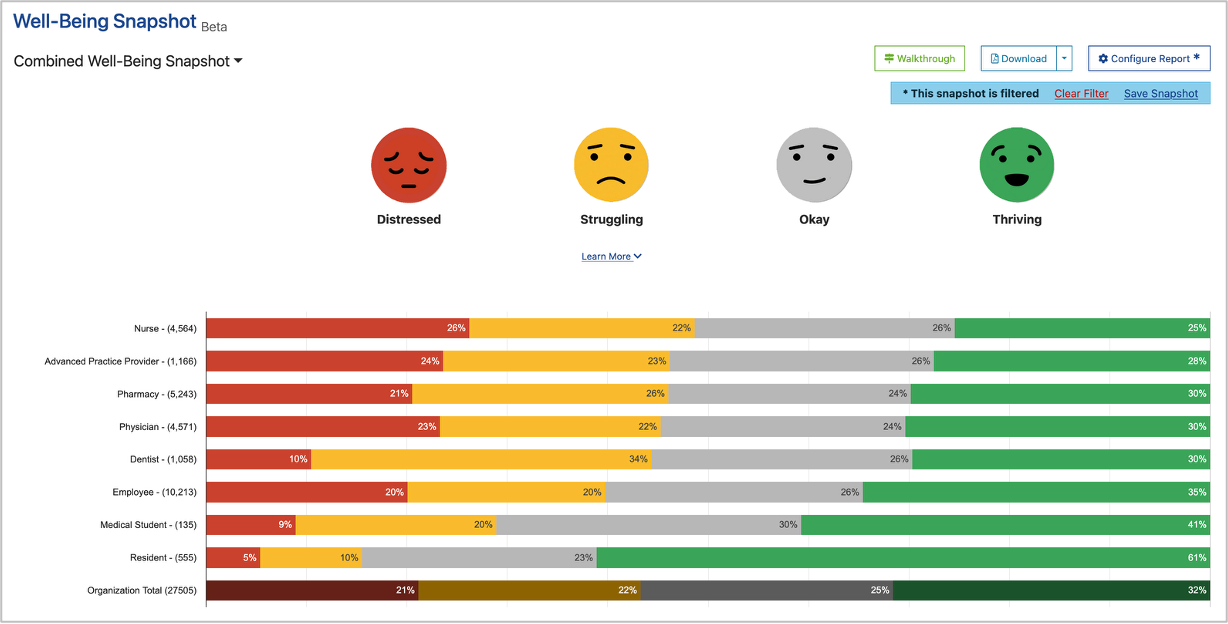
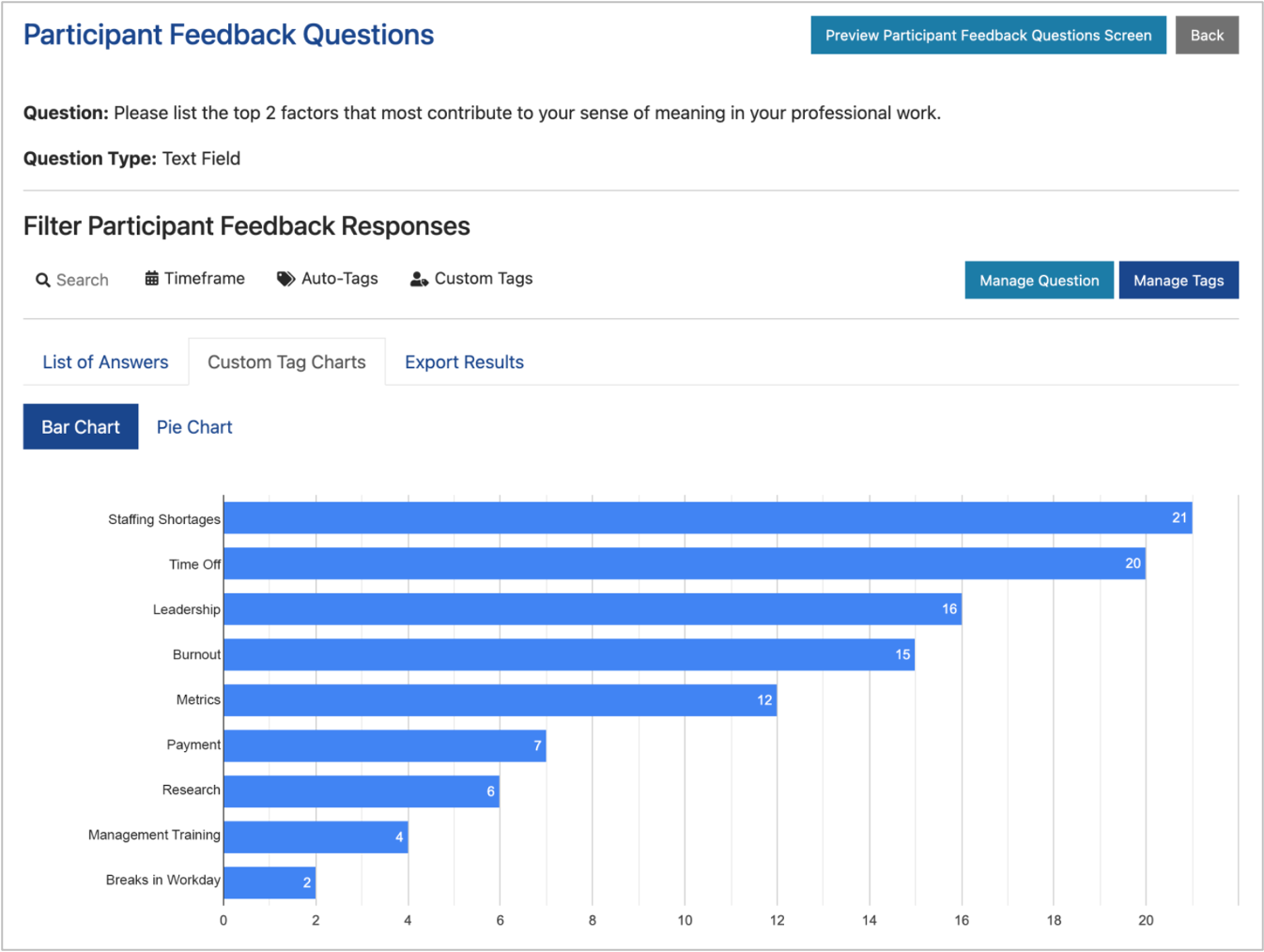
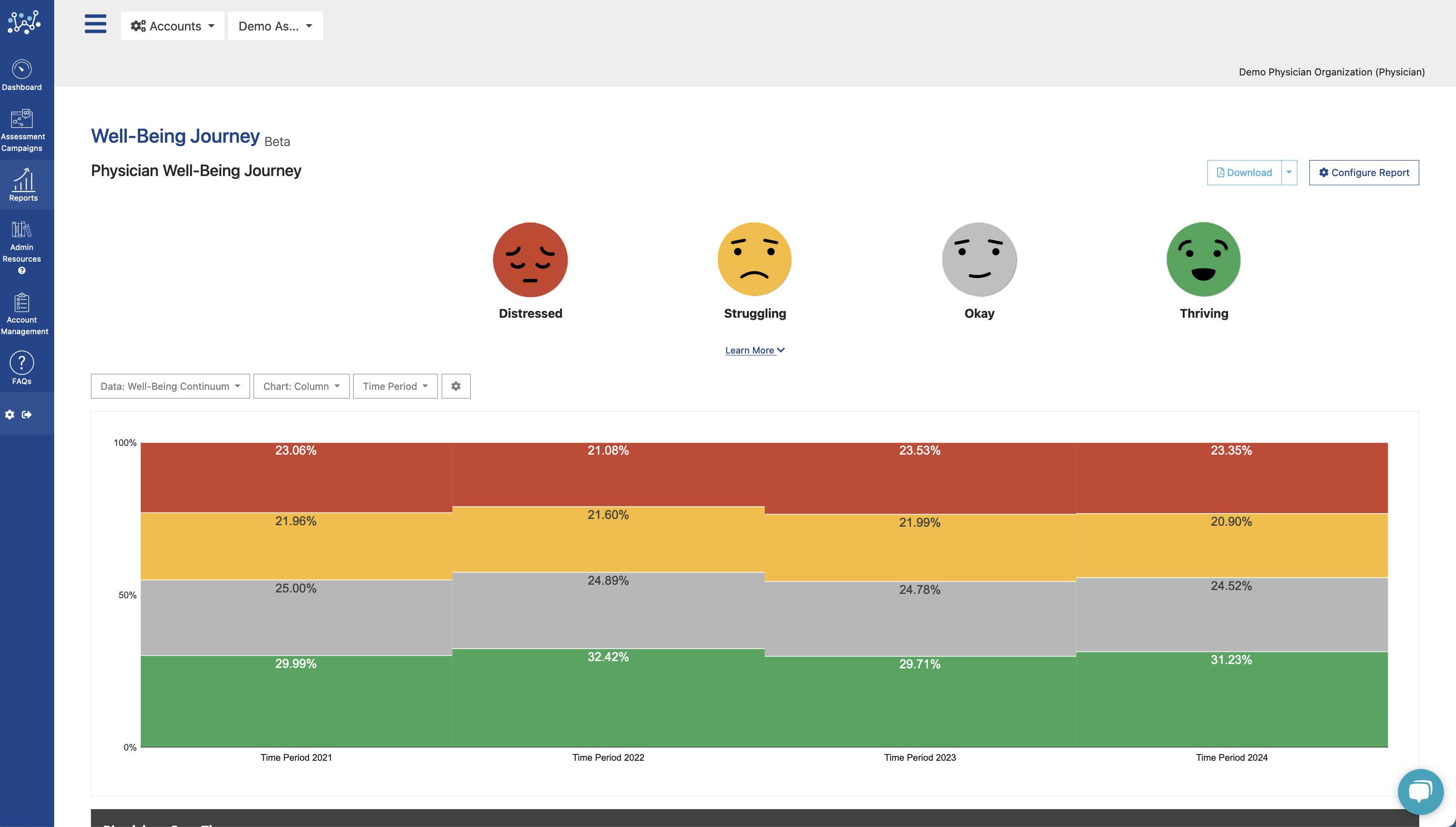
Measuring clinician burnout is an essential first step toward addressing systemic issues that can cause distress. By taking the time to assess clinician well-being and mental health, healthcare organizations can better understand the scope of the problem and develop targeted strategies to address it. Moreover, validated assessment can provide valuable insights into potential sources of distress, enabling healthcare organizations to identify and target underlying issues that may be contributing to clinician burnout. Ultimately, taking the time to assess burnout can equip healthcare organizations with the necessary data points to facilitate meaningful change.
By implementing evidence-based practices and interventions, medical professionals and healthcare organizations alike can work together toward improving clinician well-being
[RELATED: The Well-Being Assessment Tool Used By 1,000+ Healthcare Organizations]
While there is still much work to be done in this area, the research suggests that by prioritizing systemic changes and evidence-based interventions, we can make significant strides in supporting the well-being of our frontline healthcare workers.
Maximizing Clinician Mental Health
To ensure the well-being of our healthcare professionals and improve mental health outcomes, we must prioritize systemic changes and evidence-based interventions. Implementing self-assessment tools, addressing systemic drivers of distress through measurement, and taking steps to reduce stress levels are all essential components of creating a healthier work environment for medical personnel. By investing in clinician well-being now, we can help create a lasting impact on both individuals’ career satisfaction as well as positive patient outcomes.
Address the Distress
Take control of your mental health today and learn more about the Well-Being Index. With over 500,000 healthcare professionals already using the tool, the Well-Being Index is a validated and evidence-based self-assessment tool designed to help clinicians monitor and maintain their well-being. By completing the assessment regularly, clinicians can gain valuable insights into their mental health, identify potential sources of stress, and take proactive steps to reduce burnout and compassion fatigue. Furthermore, healthcare organizations can use this data to inform system-level interventions and address the root drivers of clinician distress. Start prioritizing well-being today and join the thousands of medical organizations already addressing clinician distress.