Workplace burnout among nurses and other medical professionals has been top-of-mind for healthcare leaders in the past few years. Hundreds of institutions around the world have implemented strategic initiatives at their organizations to address distress and support the mental health of their nursing staff. But are these efforts working?
In this article, we highlight the latest data regarding nurse burnout from a wide variety of sources-including Well-Being Index assessment results from nearly 20,000 nurses last year-to answer the question: Is nurse burnout getting worse?
Latest Insights Regarding Nurse Burnout
As awareness of the epidemic of professional burnout has increased throughout healthcare, so too has research regarding its causes and impact. Recent findings of a thorough literature review published in Gavin Publishers concluded that burnout among nurses leads to chronic occupational stress, including three aspects, “emotional exhaustion, depersonalization, and feelings of low personal accomplishment on the job.”
This chronic occupational stress stemming from burnout is deeply impacting our nursing staff, causing mental health crises and even forcing thousands to leave the profession entirely. A new study by the nursing agency IntelyCare found that more than 33% of the 188,000 new nurses who graduate every year in the United States leave the bedside by the second year due to burnout. Furthermore, of the nurses that leave their profession due to exhaustion, 54% cite mental health factors like emotional toll as the culprit.
Burnout is also associated with depression. A study published in the November 2021 issue of the American Journal of Nursing found that at least 35% of nurses experiencing burnout had symptoms of depression. It was also found that nurses are more likely to experience depression than other healthcare occupations. In fact, compared to other health professionals, nurses have twice the rate of depression when burnt out.
New Nurse Well-Being Index Assessment Data
Every year, thousands of nurses and other healthcare professionals use the Well-Being Index to measure their well-being, access resources to help improve their mental health, and provide anonymous insight to their leaders to help combat the causes of distress. Since 2019, this anonymous wellness data has also been made available to the public through Well-Being Index Insights. The annual reports referenced in this section are all available for free download.
In the 2019-2020 State of Well-Being Report, over 3,800 nurse assessments were collected. Of these nurse assessments, 52.2% reported burnout. The 2020-2021 State of Well-Being Report showed an alarming increase in the already high level of nurse burnout. This report found that, of over 10,200 nurse assessments taken, 64.8% reported burnout.
To give context to the findings of the 2020-2021 report and examine any effect the pandemic had on medical professionals over this time period, a subsequent survey of Well-Being Index participants was conducted, titled the COVID-19 Impact Report. This report provided further insight into the increase in nurse burnout. Among all other healthcare occupations featured in the report, nurses were the most likely to experience high levels of distress due to increased workload caused by the COVID-19 pandemic. The report also found that whether they were directly involved in COVID-19 patient care or not, nurses were the most likely occupational group to experience high levels of distress from March-August of 2020.
The 2021-2022 State of Well-Being Report revealed that nurse burnout levels have remained high. Of nearly 29,000 nurse Well-Being Index assessments collected, 63.7% reported burnout. In February of 2023, the latest State of Well-Being Report was published. These most recent numbers, highlighting insights from nearly 20,000 nurse assessments, show that over 60% reported burnout from their work and over 65% reported emotional problems such as feeling anxious, depressed, or irritable. The data also shows us that younger nurses were more likely to experience a high level of distress than their older peers.
[RELATED: Empowerment: The Key to Healthy Nurses]
A Path Forward
Despite the recent increase in the understanding of mental health issues affecting medical staff and the need for wellness programming, nurse burnout has remained dangerously high if not increased over the past several years.
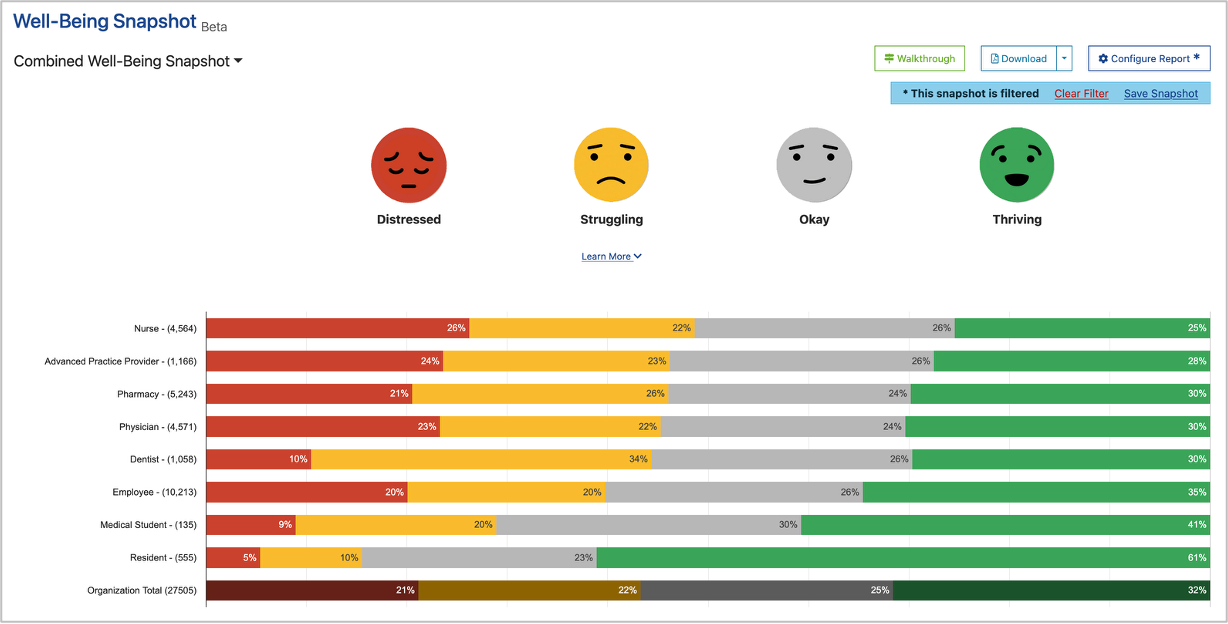
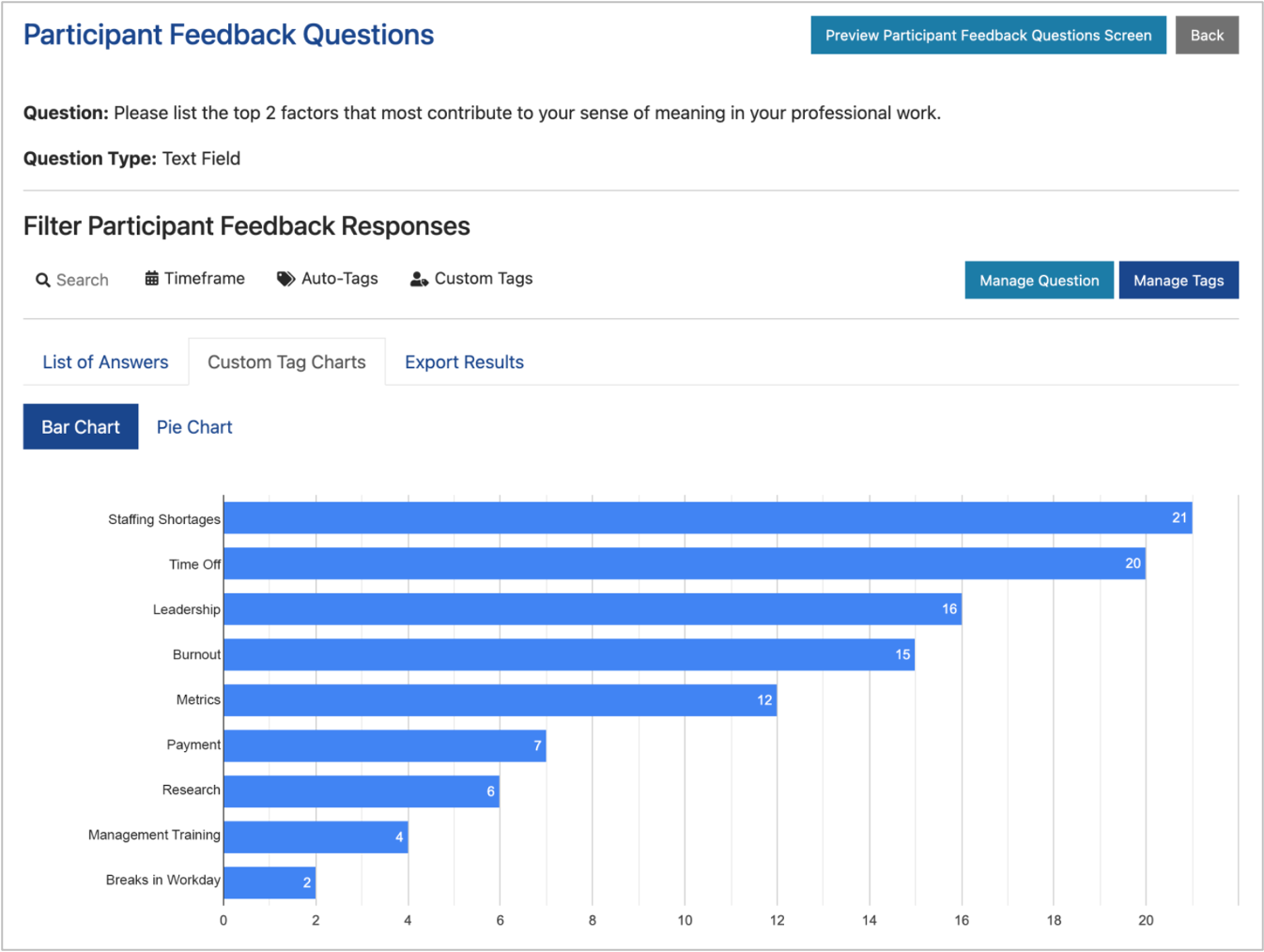
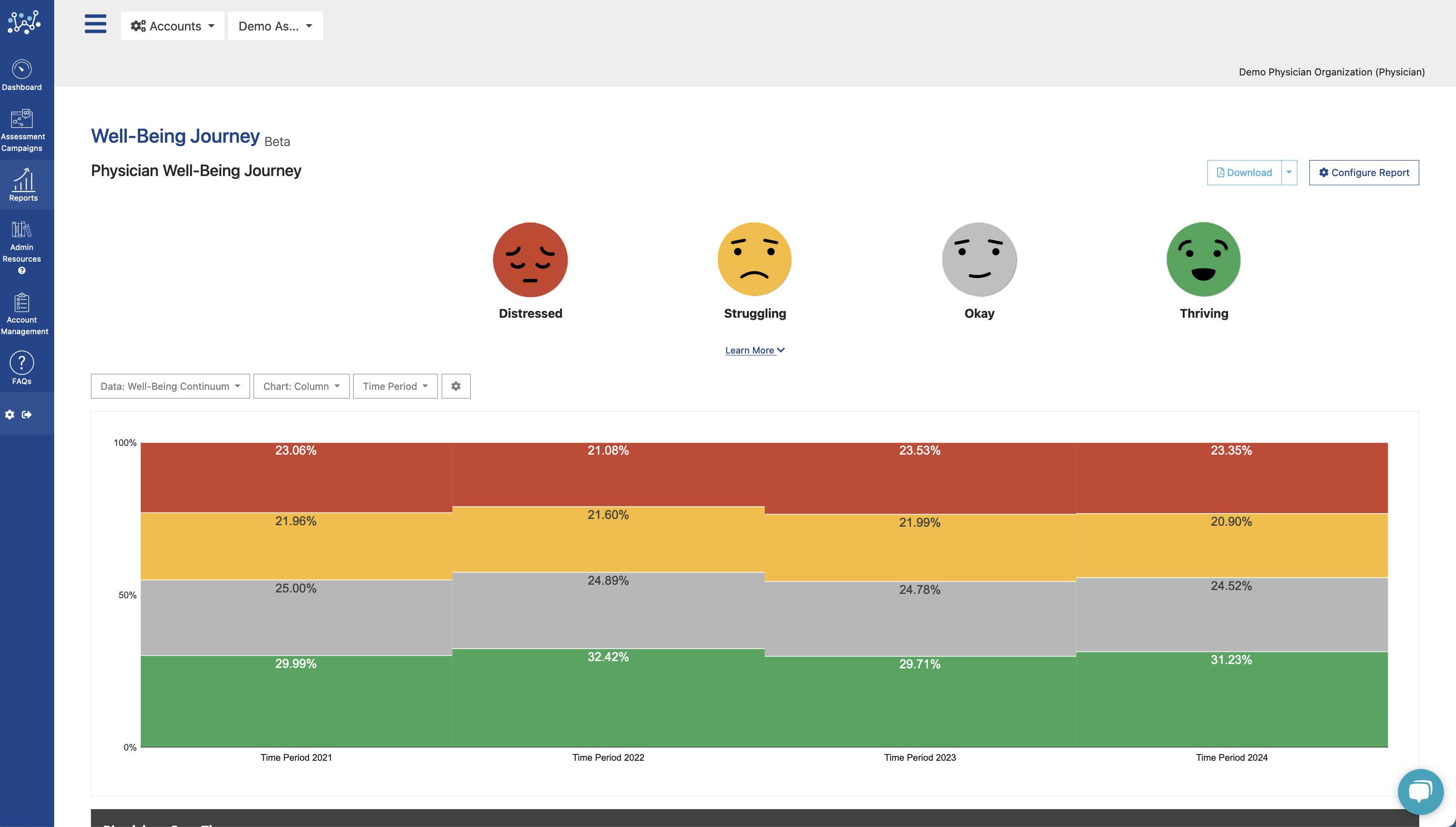
To combat these unprecedented levels of workplace distress impacting our healthcare professionals, organizational leadership must re-examine their wellness efforts to ensure that strategic initiatives in place, if any, are the most effective they can be. This starts with a data-driven and evidence-based approach. To identify the true causes of nurse burnout, institutional leadership needs department-level data regarding the well-being of staff.
For over ten years, healthcare organizations around the world have turned to the Well-Being Index to provide this insight, along with baseline measures to compare their groups’ wellness to national averages. The validated Well-Being Index assessment was invented by Mayo Clinic to deliver the data and tools leaders need to make real, measurable change in the mental health of medical staff. For more information on how institutions like yours utilize the Well-Being Index to spark change, visit our case studies, frequently asked questions, or take a free demo of the revolutionary tool.
Together, we can Go Beyond Burnout.