Healthcare provider burnout has reached crisis levels across all clinical roles, but the experience of burnout varies significantly between physicians, nurse practitioners (NPs), and physician assistants (PAs). While physicians have historically been the focus of burnout research and interventions, nurse practitioners and physician assistants face their own unique pressures that contribute to distress. Understanding how provider burnout manifests differently across these roles is essential for healthcare leaders developing targeted wellness strategies that address the specific needs of their entire clinical workforce.
What Is Provider Burnout and Why Does It Matter?
Provider burnout is a state of chronic workplace stress characterized by emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. This occupational phenomenon affects healthcare professionals’ ability to provide safe, quality patient care and contributes to significant organizational costs through turnover, reduced productivity, and increased medical errors. The consequences extend beyond individual clinicians to impact patient outcomes, safety, and the financial stability of healthcare organizations.
Provider Burnout Rates: How Physicians, NPs, and PAs Compare
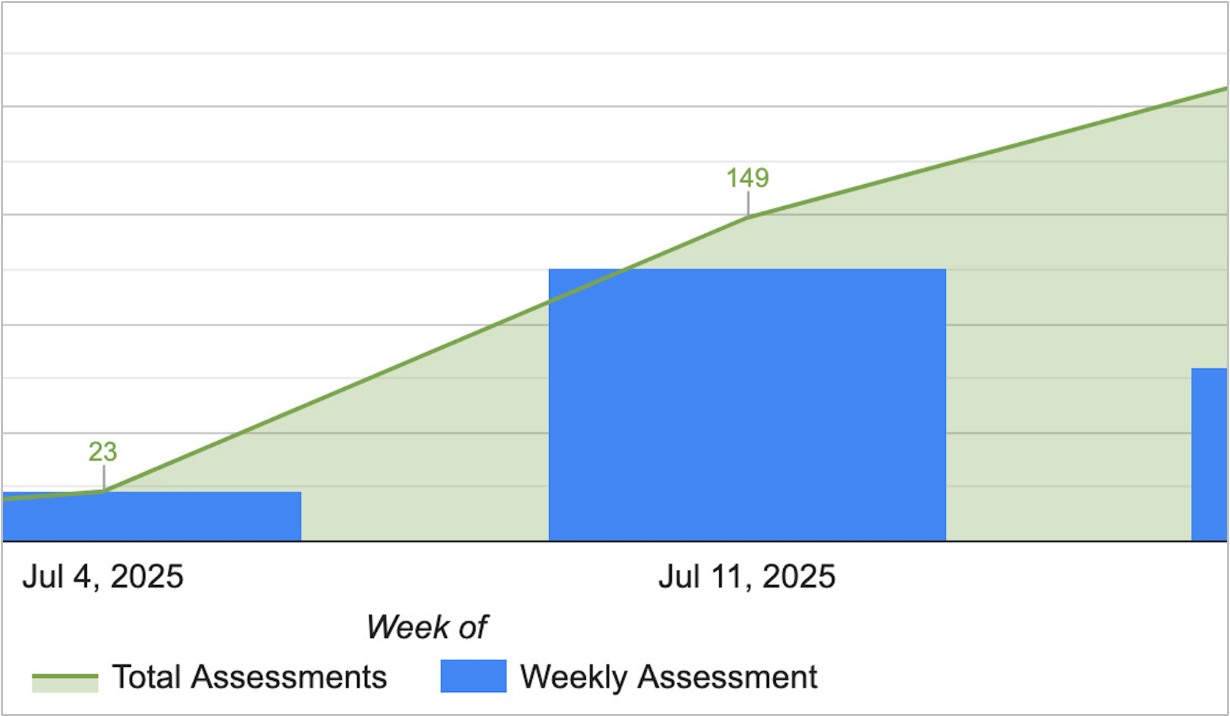
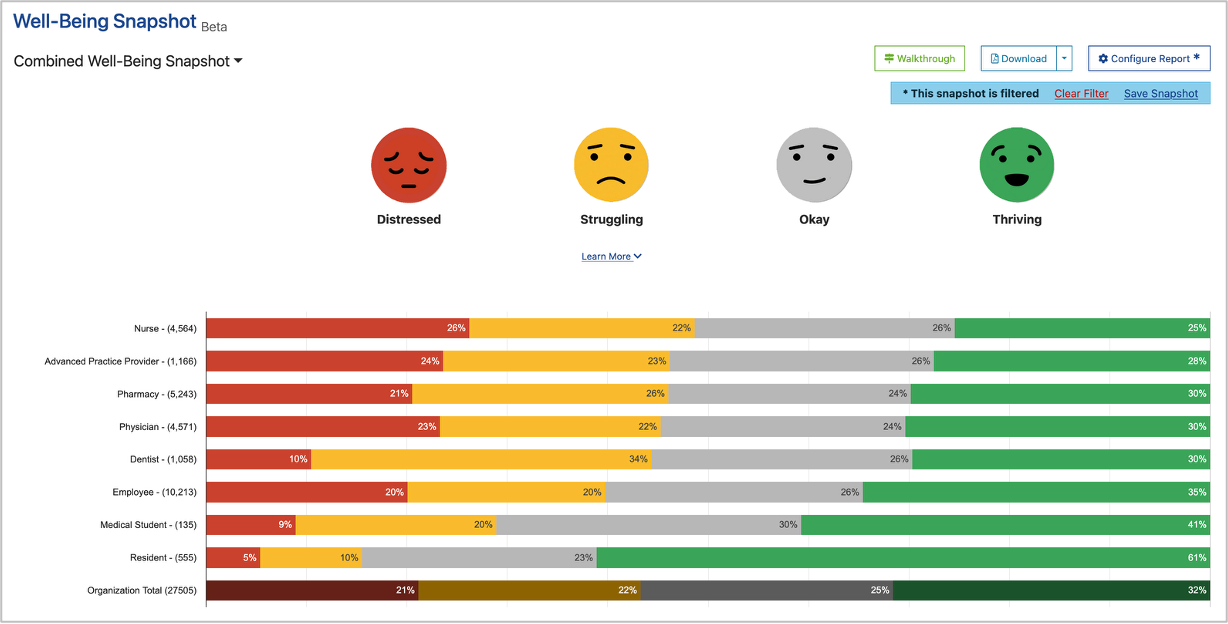
Data gathered using validated assessments reveals important differences in burnout prevalence across provider types. These most recent statistics show that advanced practice providers experience burnout at rates that demand attention from healthcare leadership.
The Well-Being Index has been validated to identify distress and stratify well-being specifically in nurse practitioners and physician assistants, making it possible to accurately measure and compare burnout across provider roles. This validation enables organizations to track meaningful differences and implement role-specific interventions.
Key findings from well-being research show:
- Physicians consistently report high burnout rates, with significant variation by specialty and practice setting
- Nurse practitioners face unique stressors related to scope of practice limitations and role ambiguity
- Physician assistants experience burnout influenced by their collaborative practice requirements and organizational positioning
Unique Burnout Drivers for Physicians
Physicians face several distinct contributors to burnout that stem from their training, regulatory environment, and clinical responsibilities:
Administrative burden and documentation requirements. Physicians spend extensive time on electronic health record documentation, prior authorizations, and administrative tasks that pull them away from direct patient care. This burden has consistently emerged as a top driver of physician distress.
Malpractice liability and risk. The threat of litigation creates constant psychological pressure that affects clinical decision-making and contributes to defensive medicine practices.
Specialty-specific pressures. Different medical specialties face varying burnout risks based on factors like patient acuity, call schedules, procedural demands, and patient volume. Emergency medicine, family medicine, and internal medicine consistently show elevated burnout rates.
Loss of professional autonomy. Increasing organizational consolidation and standardized protocols have reduced physician control over practice conditions and clinical decision-making.
[RELATED: The Business Case for Physician Well-Being: how funding wellness can future-proof your finances]
What Makes NP Burnout Different
Nurse practitioners experience burnout driven by factors unique to their professional role and scope:
Scope of practice restrictions. Variability in state regulations regarding independent practice authority creates frustration and limits professional autonomy. NPs in more restrictive states often report higher distress related to practice limitations.
Role ambiguity and identity. Nurse practitioners sometimes struggle with professional identity as they navigate between nursing and medical models of care, particularly in settings where their role is poorly defined or understood.
Workload and patient expectations. Many NPs carry patient panels comparable to physicians while also managing care coordination responsibilities traditionally associated with nursing roles.
Limited organizational recognition. In some healthcare systems, NPs face challenges gaining equal recognition for their contributions compared to physician colleagues, affecting both compensation and professional satisfaction.
PA-Specific Burnout Contributors
Physician assistants face their own set of burnout risk factors shaped by their collaborative practice model:
Dependent practice requirements. Unlike some NPs who can practice independently in certain states, PAs must maintain supervisory relationships with physicians. This structural requirement can create stress when supervision is inadequate or when organizational systems don’t support effective collaboration.
Role flexibility challenges. While PAs are trained as generalists who can transition between specialties, frequent role changes or unclear expectations can contribute to stress and burnout.
Career advancement limitations. The PA profession offers fewer formal advancement pathways compared to physician careers, potentially contributing to reduced professional fulfillment over time.
Compensation concerns. Despite comparable workloads, PAs often face pay disparities compared to NPs and physicians, contributing to feelings of being undervalued.
Common Threads: Shared Burnout Drivers Across Provider Types
Despite role-specific differences, physicians, nurse practitioners, and physician assistants share several common burnout contributors:
- Excessive workload and time pressure affecting all clinical roles
- Electronic health record burden creating documentation stress universally
- Lack of organizational support for well-being across provider types
- Patient complexity and acuity increasing demands on all clinicians
- Work-life integration challenges affecting personal relationships and health
- Inadequate staffing levels forcing all providers to do more with less
- Poor leadership behaviors creating toxic work environments regardless of provider role
Research on leadership behaviors and clinician well-being consistently shows that supervisor actions significantly impact burnout across all healthcare roles.
Measuring Provider Burnout: The Importance of Validated Assessment Tools
Accurately identifying and tracking provider burnout requires assessment tools validated for specific healthcare roles. Invented by Mayo Clinic, the Well-Being Index has been scientifically validated for physicians, and separate validation studies have confirmed its efficacy for identifying distress in nurse practitioners and physician assistants.
Using validated assessment tools enables healthcare organizations to:
- Establish baseline well-being metrics for different provider groups
- Track changes over time to evaluate intervention effectiveness
- Compare well-being across roles and departments
- Identify high-risk groups who may benefit from targeted support
- Make data-driven decisions about wellness resource allocation
The Well-Being Index provides role-specific assessment and support that accounts for the unique stressors facing physicians, NPs, and PAs while allowing meaningful comparisons across provider types.
[RELATED: What Is a “Good” Well-Being Assessment Engagement Rate?]
Strategies to Address Provider Burnout Across All Roles
Healthcare organizations must implement comprehensive approaches that address both shared and role-specific burnout drivers:
System-level interventions that benefit all providers include:
- Reducing administrative burden through scribes, documentation support, and streamlined processes
- Optimizing staffing levels to match patient volume and acuity
- Implementing evidence-based scheduling that respects work-life boundaries
- Creating cultures of psychological safety where providers can voice concerns
Role-specific supports tailored to each provider type:
- For physicians: addressing specialty-specific stressors, reducing liability-related anxiety, and restoring professional autonomy
- For NPs: clarifying role expectations, advocating for appropriate scope of practice, and providing mentorship opportunities
- For PAs: establishing effective supervision structures, creating advancement pathways, and ensuring equitable compensation
Leadership development focused on behaviors that protect provider well-being across all roles. Research consistently shows that leadership behaviors significantly impact clinician burnout and satisfaction.
[RELATED: How Can I Improve the Well-Being Of My Teams? Strategies for Healthcare Leaders]
The Business Case for Addressing Provider Burnout
Investing in provider well-being makes financial sense for healthcare organizations. The economic costs of burnout include:
- Turnover replacement costs averaging hundreds of thousands of dollars per clinician
- Lost productivity from reduced clinical efficiency and increased absenteeism
- Medical errors and patient safety events with financial and reputational consequences
- Decreased patient satisfaction scores affecting reimbursement
- Recruitment challenges in markets known for poor provider well-being
Addressing burnout across all provider types creates a positive return on investment through improved retention, enhanced productivity, better patient outcomes, and stronger organizational reputation.
Taking Action: Moving From Measurement to Meaningful Change
Understanding the differences in provider burnout across physicians, NPs, and PAs is only the first step. Healthcare leaders must translate this knowledge into action by:
Starting with a validated, role-specific assessment. Use scientifically validated tools like the Well-Being Index to establish baseline metrics and identify areas of greatest need across your provider workforce.
Analyzing data by role. Look for patterns that reveal whether certain provider types face elevated burnout risks in your organization. Compare findings to national benchmarks available through the State of Well-Being reports.
Implementing targeted interventions. Design wellness initiatives that address both common stressors affecting all providers and role-specific challenges facing physicians, NPs, and PAs differently.
Tracking progress over time. Regular assessment allows you to measure whether interventions are working and make data-driven adjustments to your wellness strategy.
Engaging providers in solutions. Include physicians, nurse practitioners, and physician assistants in designing and implementing wellness initiatives to ensure interventions address their actual needs.
[RELATED: 4 Steps to Promote Professional Well-Being in Medicine]
Conclusion: A Comprehensive Approach to Provider Well-Being
Provider burnout is not a one-size-fits-all problem. While physicians, nurse practitioners, and physician assistants share many common stressors, each role faces unique challenges that require tailored solutions. Healthcare organizations that recognize these differences and implement comprehensive, role-specific interventions will be better positioned to support the well-being of their entire clinical workforce.
The first step toward meaningful change is accurate measurement. By using validated assessment tools that account for the distinct experiences of different provider types, healthcare leaders can identify specific areas of concern and track the effectiveness of wellness initiatives over time.
Ready to understand provider burnout patterns in your organization? The Well-Being Index offers validated assessment tools for physicians, nurse practitioners, and physician assistants, giving you the data you need to create targeted wellness strategies. Request a demo to see how measurement-driven approaches can transform provider well-being across all clinical roles.