The American Heart Association (AHA) has recently highlighted the fact that nurses have a 14 percent higher-than-average incidence of poor cardiac health due to job stress. This statistic is just one example of the many adverse consequences of nurse burnout and distress. Here’s what the research has to say about the causes of distress in the nursing profession, and how organizational restructuring and empowerment can improve nurse wellness.
Why are nurses especially subject to work stress?
The nursing position has been recognized as a stressful job role for many years. Research on stress and burnout in the nursing profession cites “physical labor, human suffering, work hours, staffing, and interpersonal relationships” as contributors to distress, along with the “increasing use of technology, continuing rises in health care costs, and turbulence within the work environment” that have taken place in more recent years. Burnout, defined as “a syndrome characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment,” is not the only dimension of nurse distress, however. In fact, there are six dimensions of distress and well-being that impact nurses in their professional and personal lives, including severe fatigue, work-life integration, suicidal ideation, and more.
[RELATED: The Current State of Nurse Well-Being in the US]
The Symptoms of Nurse Distress
It may seem obvious that having healthcare facilities staffed with highly distressed nurses is not a good situation—but many don’t realize the full impact and devastating symptoms of distress on the nurses themselves, the patient, and the organization.
- Increased illness: The immune system’s response to stress leads to increased illness, which in turn leads to absence and staffing problems on nursing teams causing even more distress.
- Higher turnover: Hiring and orienting new nurses is time-consuming and expensive, and it also creates a drain on an organization’s more experienced staff.
- Worse patient outcomes: Studies show that mortality and morbidity rates are higher among patients of overburdened nursing staff. Poorer caring behaviors also occur, as overstressed nurses simply aren’t able to perform at their normal capacity.
How Empowerment Reduces Distress
Multiple studies over the years indicate that an empowered role at work is associated with less job tension, more engagement, better outcomes, and a strong positive feeling about one’s work.
What does an empowered work environment look like?
Empowerment requires support by leadership that is “inclusive, non-authoritarian, visionary, and emotionally intelligent,” according to an article published in Nursing Management. It is nurtured by an environment of safety, in which nurses can initiate changes that will help them perform more effectively. Or, as the article succinctly phrases it, “Nothing about me without me.”
Leveraging Structural Empowerment
According to Martie Moore, RN, CNO of Medline Industries, “Nurse empowerment largely hinges on the infrastructure and communication design of an organization.”
Changing your management structure to prioritize staff empowerment is the best approach, because then your long-term sustainability isn’t dependent on one particular staff member’s leadership skills. Nursing Management defines an empowering structure as one which supports “shared team governance, open leadership communication, and supportive and empathetic nursing team relationships.” Shared governance, according to a continuing education course at Nurse.com, consists of “teams of nurses who are self-managed, autonomous in problem solving, and are decision makers for patients and nurses.”
Relief Comes From the Top Down
Leaving nurse distress unaddressed is a failure of management that not only endangers the lives of providers but also has a direct effect on quality of care and patient safety. Moving forward, healthcare organizations must understand the current state of their nurses’ well-being and enact systemic changes such as those described above in order to reduce the negative impacts of distress on both the individuals and the institutions.
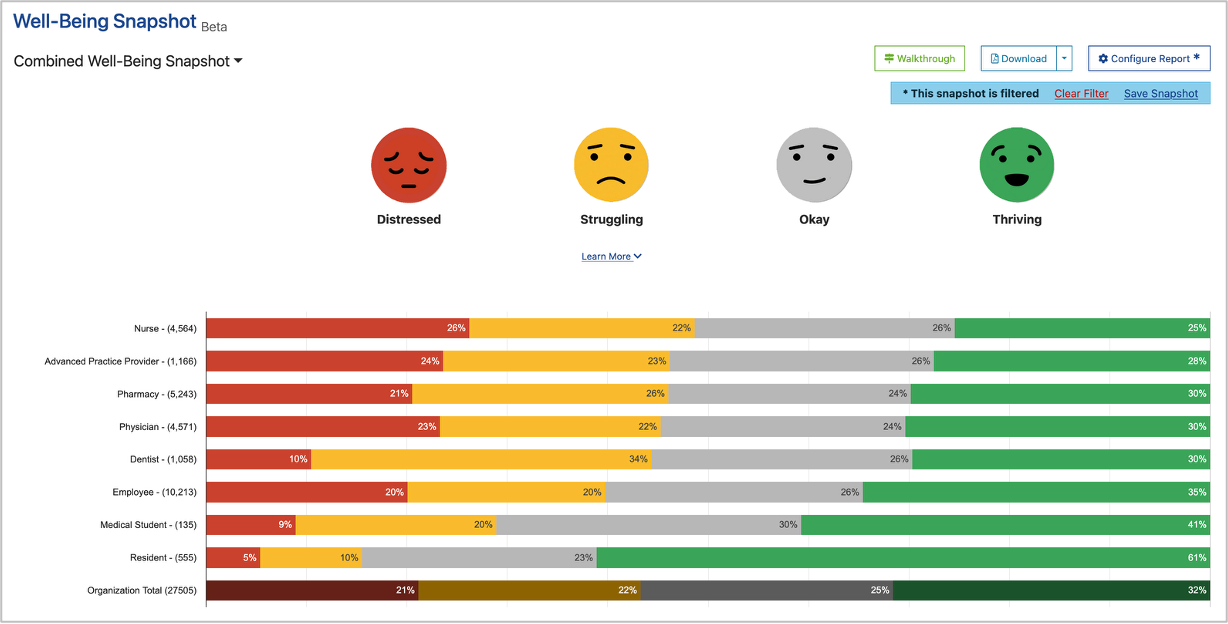
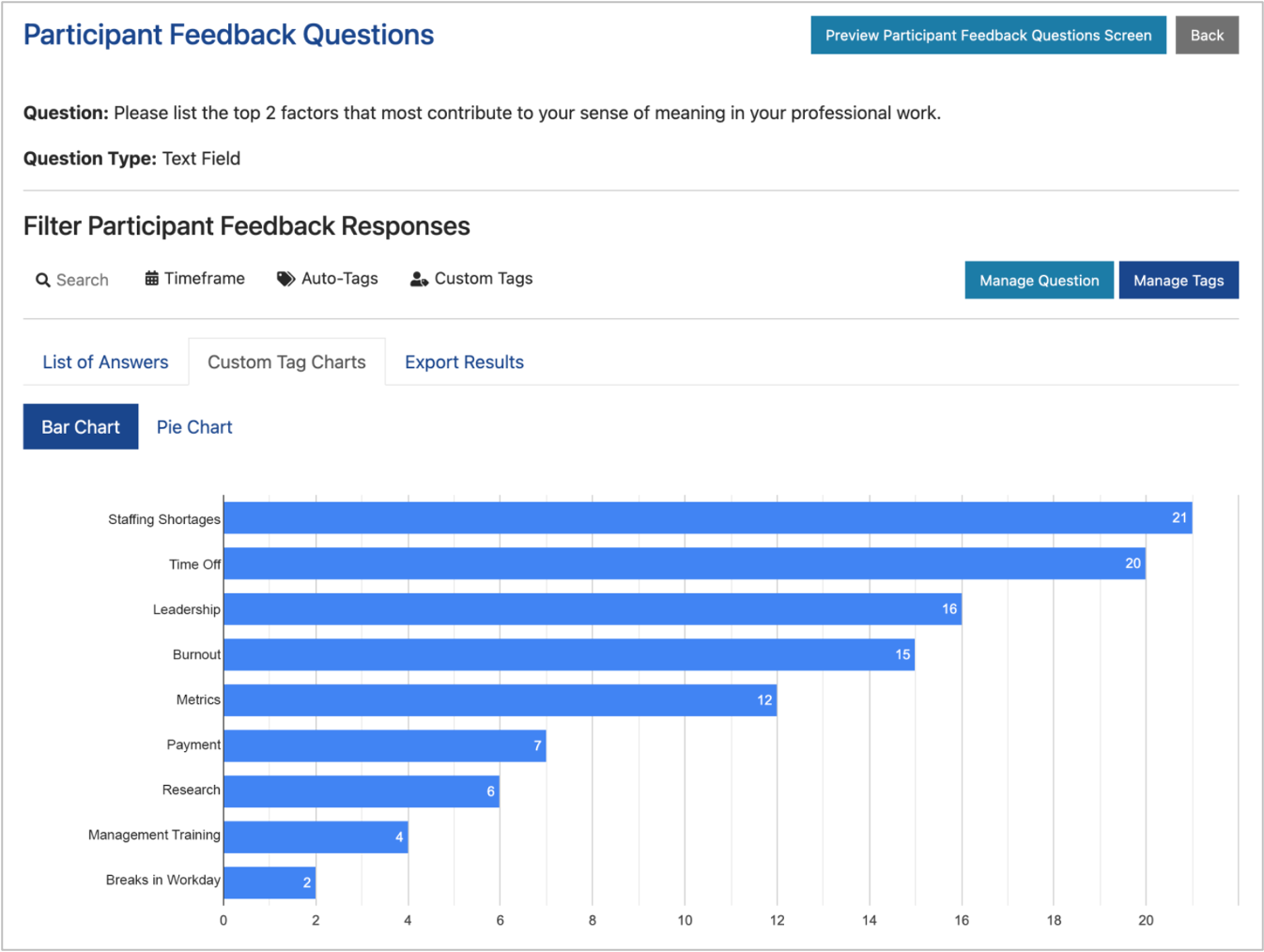
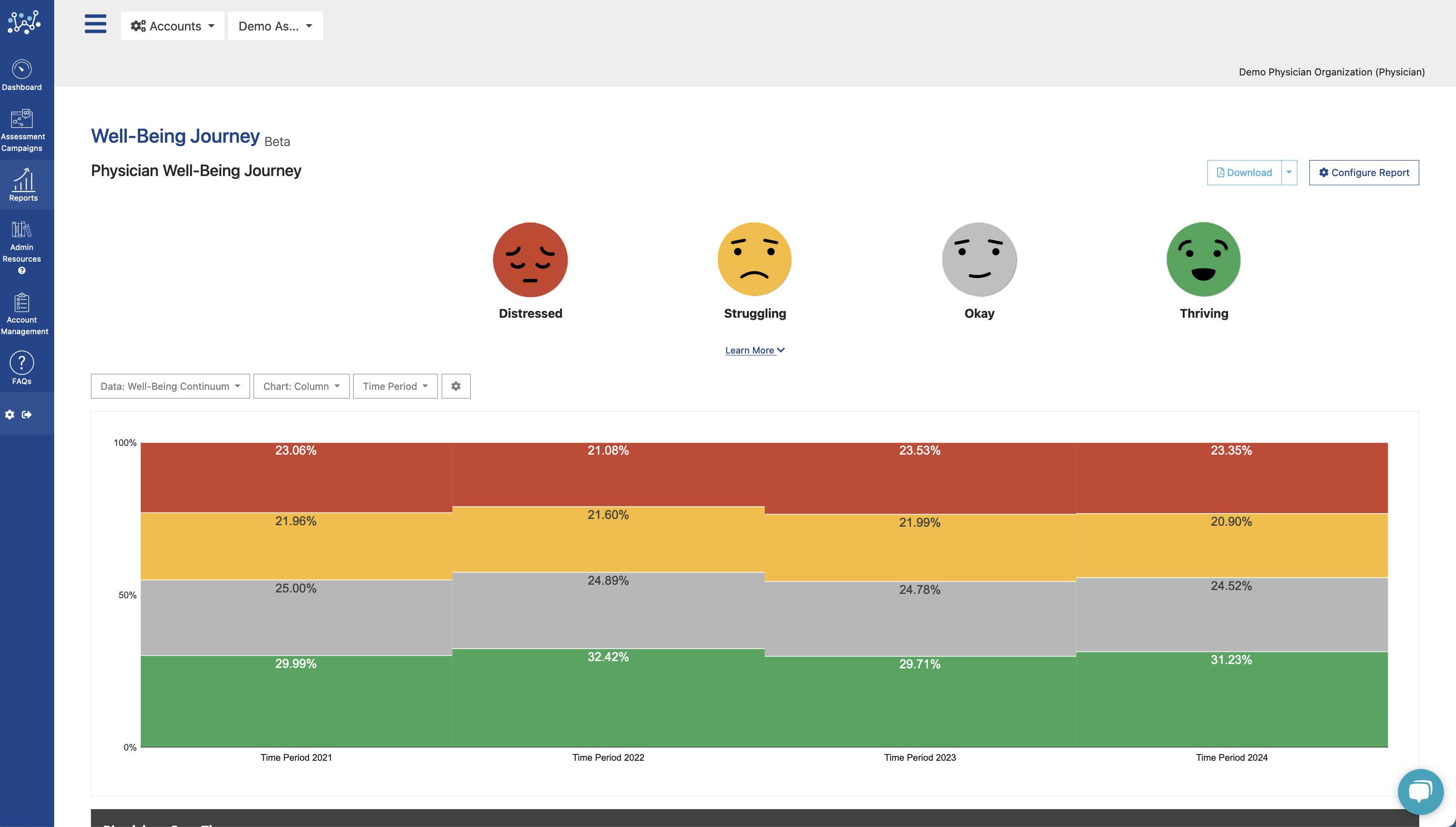
The Nurse Well-Being Index gives you a window into how every member of your nursing staff is doing. It also gives you an analytic baseline, allowing you to evaluate the effectiveness of the empowerment measures that you put into place.